Getty Images
At theRadiological Society of North America’s (RSNA) 2021 annual meeting in December,James Brink, MD, FACR,Radiologist-in-Chief atMassachusetts General Hospital, in Boston, Mass., and a Juan M. Taveras Professor of Radiology withHarvard Medical School, led a Plenary Session titled “Radiology in the Value-based Healthcare Arena: Player or Pawn?” There is no doubt that the concept of value is an ever-present thought in the mind of Brink. He likes to consider value in terms of the consumer industry, which he did often during theCOVID-19pandemic when he would engage with his children and their families, at various locations around the globe, playing Mario Kart and Nintendo together on Sundays to stay connected. The value of that product increased in their view, as it allowed for a global experience.
价值最好由相对于成本的体验质量来定义。他指出,准确的诊断和精确的测量是质量的关键,及时便捷的服务和综合护理是质量的关键。
放射学在价值方程中意味着什么?
He referenced a paper on “Radiology at the Helm of Value-Based Care Transformation: From Stewardship to Leadership.” Published in theJournal of the American College of Radiology(JACR) byPamela Johnson, MD,Johns Hopkins Health Center, with YoshimiAnzai, MD, MPH,University of Utah Healthcare, offered this: “Radiology is at the epicenter of medical care and delivery, and radiologists are well-suited to coordinate care transformation even outside of our immediate specialty.”
“If we don’t actually engage as players in this value-based healthcare arena then other specialties and other organizations will be looking to define their role and we may become pawns in their initiatives, so it behooves us to participate as thoroughly and vigorously as we can,” said Brink.
He noted insights delivered several years ago byVivian Lee, MD, PhD, MBA, who gave an oration on driving value for imaging, where she said. “Radiologists must cement our value as the stewards of timely and accurate diagnoses; must be actively engaged core members of the care team. She added that the best measures of accurate and timely diagnoses must be embraced, and that transparency in these quality measures can accelerate transformation.”
Elevating the Value of Imaging
Answering the question of “How do we elevate the value of our practice?” calls first for looking at how we eliminate low value imaging.
He was intrigued by theJAMA2021年初的观点,低价值护理被定义。它提出需要克服组织文化,以消除低价值的关怀。他指出,有必要制定政策和干预措施,通过关注偏见来调整动机,并补充说,行业应避免膝跳反射行为。
Notably, the pandemic did not make this easy. He offered, “We feel like our practice is crushed with enormous work burden, as we have seen a 20-30% increase in imaging volume at MGH in this year alone,” adding, “Some of that volume growth may be related to low value exams that perhaps were not necessary. Perhaps the tool that can help eliminate low value imaging the most is decision support, on two fronts: that which is leveraged before imaging, and that leveraged by radiologists to help with most appropriate recommendations.”
布林克指出,CDS法规指出:“到2023年1月1日,医生在订购高级诊断影像检查(CT、MRI、NM和PET)时,必须通过CDS系统咨询政府批准的、循证的适当使用标准。自2020年1月1日起,目前正在进行为期3年的教育和运营测试。”
“This is an important means of eliminating low value imaging,” said Brink.
Brink noted a JAMA Viewpoint published April April 8, 2021, by Allison H. Oakes, PhD, and Thomas R. Radomski, MD, MS, on “Reducing Low-Value Care and Improving Health Care Value.” It offered, “Low-value care, defined as the use of a health service for which the harms or costs outweigh the benefits, is a pervasive and enduring problem in the US. Enacting policies that limit reimbursement for low-value services is an important step in mitigating such care.”
In order to eliminate low value imaging, there are multiple tools and considerations which Brink highlighted. Clinical Decision Support (CDS) before and after imaging; ACR Appropriateness; ACR Select, which helps eliminate low value imaging; the new legislation (effective January, 2023); and a Decision Support Tool to help guide us to recommend the most appropriate action.
Promoting High-value Imaging
“The value equation is analogous to radiology,” contends Brink, adding, ”If we do not engage as players, other specialties will and we may become pawns, so It behooves us to participate fully.”
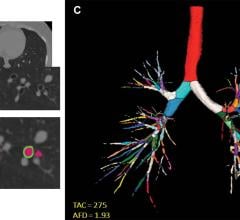
He reinforced how radiologists are continually drawing on lessons about improving quality with accurate diagnoses and precise measurements, as well as improving experience with timely and convenient service and integrating imaging care into the care continuum that the patient experiences. Addressing innovative ways to advance quality, he noted the role ofartificial intelligence(AI) in improving care, and leveraging it to radiology’s advantage is critical. He offered a deep dive into solutions, which answer the mandate for improving experiences and elevating value overall. A summary of those recommendations are presented below.
Value-based Care: Improving Experiences
Patient Engagement,by reducing missed care opportunities, and improving compliance with screening recommendations. This includes transportation assistance. Also, improving compliance with screening guidance, CT Lung Cancer Screening Initiative, including practice support and outreach, door to door visits to drive-up use of screenings.
布林克指出,在这一连续过程中,最重要的是,如果人们不能理解信息,努力就毫无意义。要解决这些问题,可以开展一项针对拉美裔社区的筛查活动,并将重点放在那些可能无法返回进行随访的脆弱患者身上。
Virtual care,实现虚拟咨询和电子咨询。他指出,特别是在大流行期间,这改变了我们与咨询医生、甚至可能与患者进行最佳互动的方式。他提到了虚拟阅览室,这是布里格姆妇女医院(Brigham & Women’s Hospital)作为流行病的副产品开发的。他补充说:“这将是未来几年的好处,因为它包括通过视频会议和屏幕分享的面对面互动,实时审查发现,为患者和转诊医生带来好处。”
Ambulatory access,which leads to improving throughput and decreasing both ED visits for imaging and length of stay in ER, which is perhaps the most important variable. Also, focusing on rads’ ability to work with other specialties to improve access to all aspects of imaging and non-imaging care.
他指出,MGH放射学项目的医疗分析小组通过进行流程挖掘、摸访急诊以及与员工和利益相关者讨论来创建统一的数据集,该数据集具有描述患者个体和急诊总体状态的特征,从而帮助急诊室缩短住院时间。机器学习模型被用来确定什么是驱动逗留时间的最重要和最具影响力的特征。基于各种人工智能预测模型,他们将这些模型组合成一个单一的预测模型(就像追踪飓风的方式一样)。这向我们展示了我们可以在哪里集中我们的优先事项来提高停留时间的长度,也给了我们一个强有力的度量来衡量我们做得有多好,并跟踪我们在寻求和实施过程改进计划时所利用的好处。缩短急诊科的住院时间有助于集中重点,并提供显示流程改进的指标。
Care coordinationis vital to ensuring seamless end-to-end care is being provided. This care coordination is such an important part — clinicians participating with care teams to make sure patients get the best care they can. He referred to this as “The Godfather of them all.”
Brink elaborated on the importance of coordinating follow-up imaging. This entails addressing radiologist recommendations collaboratively. It also ensures clinically necessary diagnostic follow up recs are followed through, executed or modified, or at least a conscious decision is made to not do anything if that is most appropriate. It requires not only dedicated IT tools but collaboration among multiple care teams.
“The cumulative impact is that this improves patient safety and quality of care,” offered Brink.
On Reducing Cost
We know cost is an important variable, Brink noted. “One thing that is universal is the site of service. We know there are lower cost alternatives to some of the high=cost options.”
He noted published reports which show efficiencies gained and cost ratios with dramatic improvement from shifting to a clinic from a hospital. “When it comes to really making this work, we have to think beyond simply being individual hospitals or individual practices, but we need to think like health systems,” reinforced Brink.
To that end, he referenced aHarvard Business Review(HBR) article, dated Jan. 24, 2019, by Jeff Goldsmith, titled “What a health system is and isn’t.” The author wisely implores our systems to consider the following: “Be an operating company, not holding companies. At its core, be a clinical enterprise, not just a collection of assets. Next, provide patients and families with a seamless and consistent experience across the health system, and lastly, affirmatively control the delivered cost of care (control needless variation with best practices provided by point of care).”
A Focus on Global Strategies
Brink addressed an important question he encourages all radiologists to consider. That is: What can we do as a profession, globally, to better position us as players in the value-based health care arena?
He credited the European Society of Radiology for convening other professional organizations who participated in the development of multi-society expert statement, “Radiology in the Era of Value-Based Healthcare,” on how we can participate in value-based health care. Published in the journalRadiology(Dec. 21, 2020), it highlights that radiologists are key members of the healthcare continuum and can contribute to moving to a value-based system. The Society expert statement included ACR, CAR, ESR, IS3R, RANZCR, and RSNA, and offered these key points:
•Value-based healthcare (VBH) is a framework for improving individual patient health outcomes per unit of expenditure.
•Radiology is a key component of healthcare, impacting greatly on patient outcomes, and must be considered a vital element of VBH.
•Embracing VBH principles, radiology can contribute to moving a value-driven system, where all investigations or interventions contribute to patient outcomes.
A subsequent viewpoint inJAMA(Oct. 6, 2020), “Radiology and Value-Based Health Care,” was written by Brink, with Adrian Brady, MB, and John Slavotinek, MB. It highlighted more specifically what need be done for radiology to be seen as a creator of value:
•Breadth of contributions to patient care we provide must be understood;
•Radiology must work to quantify our effect on outcomes;
•Clinicians referring patients for radiological studies should have accountability for their effect on the cost of medical imaging (thereby helping lower the incidence of low value care);
•Managers who plan and provide resources for health care services must understand the cost of under-supplying radiology; and
•Radiologists must actively ensure that the use of radiological investigations is justified, appropriate, and ideally, evidence based.
Imaging Value Equation
Brink closed the Plenary Session by reinforcing the Imaging Value Equation:
Value = Quality (accurate diagnoses and precise measurement) + Experience (timely, convenient service plus integrated care)/Cost (priceless)
他总结道:“如果我们工作得当,那么我们的成本将是无价的。”

Christine Book is a Contributing Editor for Imaging Technology News, and has developed a variety of content for both ITN and Diagnostic and Interventional Cardiology (DAIC). Throughout her career, she has covered radiology, cardiology and other healthcare specialties, as well as emerging trends in artificial intelligence, sustainability and Software as a Service (SaaS) technology. In addition to her editorial experience, Christine’s work has included generating national media coverage for organizations and brands, and managing marketing for multiple B2B publications.


 August 11, 2022
August 11, 2022